
Release Stored Trauma with Somatic Therapy
By focusing on sensation, movement, and nervous system regulation, somatic therapy can help shift you out of survival mode.
As researchers learn more about the lasting impact of trauma, it has become clear that trauma isn't something you can always "think your way through." On an intellectual level, you might understand that you're no longer in danger, yet you may still experience panic attacks, hypervigilance, or emotional numbness. Your mind knows that you're safe, but your body is stuck reliving the traumatic event over and over.
In fact, the prefrontal cortex—the part of your brain associated with awareness and conscious decision making—can go partially offline during traumatic activation, while more primitive parts of your nervous system take over (Kearney & Lanius, 2022; Brom et al., 2017; van der Kolk, 2015). These primitive parts developed long before we had language to describe or process our experiences.
Somatic therapy, aka body-first therapy, recognizes that trauma can leave physical imprints that need physical healing strategies. By focusing on bodily sensations and nervous system regulation, a somatic therapist can help you disrupt the body's trauma-response cycle and improve your capacity to be present in your everyday life.
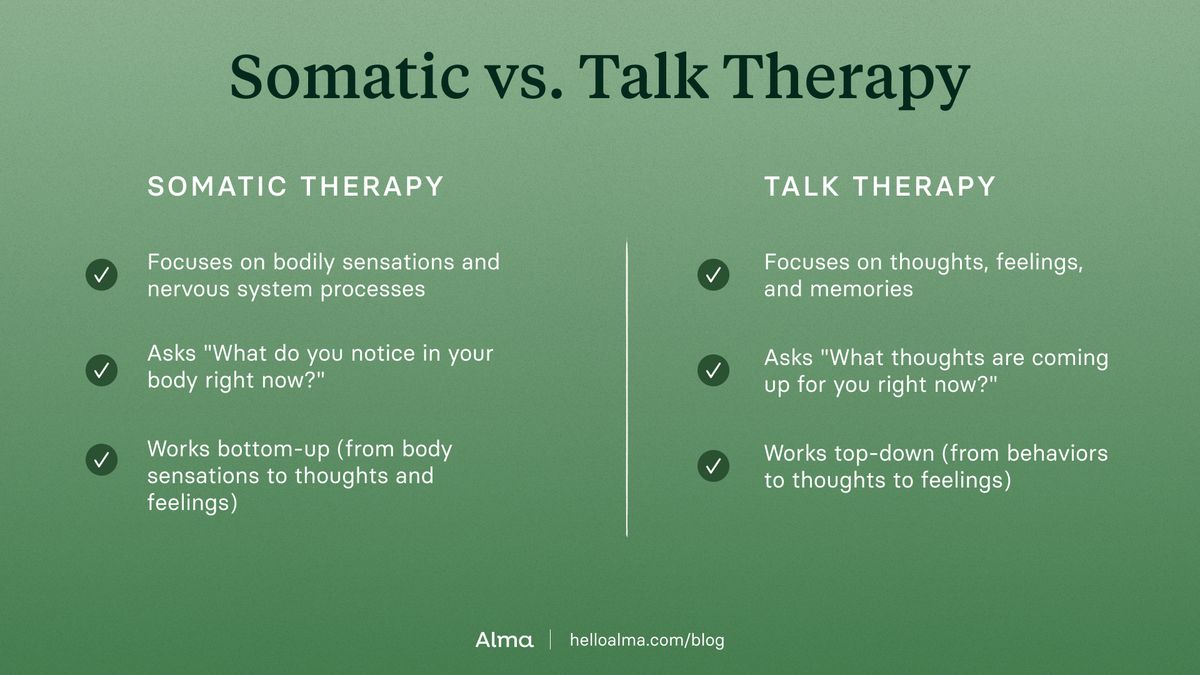
Somatic therapy vs. talk therapy
Talk therapy focuses on thoughts, feelings, and memories; somatic therapy focuses on bodily sensations and nervous system processes. Talk therapy asks "What were you thinking?" while somatic therapy asks "What do you notice in your body right now?" Talk therapy works top-down (from behaviors to thoughts to feelings); somatic therapy works bottom-up (from body sensations to thoughts and feelings). Both approaches can help, but they're addressing different aspects of the problem.
This isn't an either/or; many people use somatic therapy alongside talk therapy for deeper integration. Talk therapy provides context and meaning-making, while somatic therapy provides embodied processing and nervous system regulation. When you combine them, you get insight AND embodied change with understanding AND regulation.
Trauma lives in multiple dimensions (cognitive, emotional, relational, AND somatic) so comprehensive healing needs to address all of these areas.
How trauma becomes a nervous system pattern
Fundamentally, here’s what’s happening after you experience a trauma—your body's threat-detection system activates survival responses to keep you alive. Those survival responses are: fight, flight, freeze, fawn, or flop. They are not conscious choices but rather automatic, hardwired protective mechanisms that kick in faster than conscious thought.
In a moment of danger, this system can be brilliant; it can mobilize energy, enable you to respond, and then discharge that activated energy once the threat passes. However, when the threat is overwhelming, inescapable, or happens repeatedly, that survival response doesn't get to complete.
When the survival response is not completed, the body gets stuck in a pattern of expecting danger, even when the actual threat is long gone.
How this manifests:
- constantly scanning for threats (hypervigilance from fight/flight)
- perpetual numbness and disconnection (freeze response)
- chronic people-pleasing (fawn)
- or complete shutdown when stressed (flop)
It’s easy to mistake these things as personality flaws. They’re not. They're nervous system patterns that were once protective but have outlived their usefulness.
The research on stored trauma
Research over the past couple decades has fundamentally transformed how we understand trauma storage. We now know that traumatic experiences create what we call implicit or procedural memory, which is stored in the nervous system, fascia, and muscles (van der Kolk, 2015).
A client might not consciously remember childhood trauma details, but their body remembers through chronic shoulder tension, jaw clenching, chest tightness, or unexplained lower back pain. Once a client shared, I just can’t say what, but I know deep in my body something bad happened to me. I ache all the time. I don’t feel safe. I can’t trust anyone, even if they haven’t given me a reason not to.
Unfortunately, the body keeps holding these patterns even when explicit memory fades. And, traditional medical approaches often find nothing "wrong" because they're looking for structural damage rather than recognizing nervous system patterns.
To release these patterns, the body needs interventions that speak the language of sensation, movement, and nervous system regulation.
4 Somatic therapy techniques that release trauma
1. Body Awareness and Sensation Tracking
Before clients can release anything, they need to develop interoception or the ability to sense what's happening inside their bodies. Many trauma survivors have disconnected from their bodies because being connected doesn’t feel safe (Baranowsky & Gentry, 2023; van der Kolk, 2015).
Somatic therapists teach clients to notice where tension shows up in their bodies. Before there can be change, they have to notice the trauma still exists. Regulation comes from tracking those sensations without getting overwhelmed.
When clients can observe "oh, there's that familiar tension" rather than being consumed by it, they're creating space between the sensation and the survival response. It is in that space, that choice lives. For example, your therapist might ask something like, “Before we begin today, let’s do a body scan, listening closely to what your body is telling you today. Notice where your trauma might be showing up physically.”
2. Titration and Pendulation
Titration means working with trauma material in small, manageable amounts (like adding drops rather than dumping the whole thing in at once). It’s about gradually approaching stressful material without overwhelming the nervous system.
Pendulation is the natural rhythm of moving between activation and settling, between discomfort and resource. We touch on a difficult memory briefly, notice the activation, then deliberately shift attention to something neutral or positive like a pleasant memory or an area of the body that feels okay. The back-and-forth movement teaches the system: "I can touch this painful place AND I can come back to safety."
Over time, the body develops more flexibility and the window of tolerance expands (Baranowsky & Gentry, 2023; van der Kolk, 2015). Something I often say to clients in session to prepare them is “Let’s practice revisiting that difficult memory while you are here in a safe space.”
3. Grounding Practices and Breathwork
Both Grounding and Breathwork are the techniques that send safety signals to the nervous system (Baranowsky & Gentry, 2023; van der Kolk, 2015).
Grounding might include feeling feet on the floor, pressing hands together, orienting to the present environment, using temperature, or engaging the senses. They are distraction techniques that activate specific neural pathways that tell the brainstem "you're here, you're now, you're safe."
Breathwork is particularly powerful because breath bridges voluntary and involuntary nervous system control. For example, extending the exhale activates the parasympathetic "rest and digest" system – a longer exhale stimulates the vagus nerve, which signals safety to the entire system. Your therapist can teach you many different ways to practice breathwork so that you can find the one that works best for you.
4. Somatic Experiencing (SE)
Developed by Peter Levine, SE is built on observations of how animals in the wild release trauma naturally. When a survival response cycle gets activated but can't complete that energy gets trapped in the body; SE aims to help that trapped survival energy discharge and complete those interrupted protective responses. This means instead of just talking about what happened, SE enables clients to actually finish what their bodies started during the traumatic event.
This will look differently for each client and their specific trauma response. For example, for someone experiencing a fight response to an event where they could not fight back, the therapist might ask them “What do your hands want to do right now?” And the client might respond with wanting to push or make a fist. The therapist encourages this movement in session in a nonaggressive way as an outlet to physically say no in a controlled safe environment.
For someone experiencing a freeze response to an event where their body is completely frozen during the event, the therapist might ask them, “Do you see your legs trembling? Can you resist the urge to stop them? Can you now shake them with intention? The client shaking their legs in session vs trying to control the involuntary response is now allowing their body to finish the cycle and start to heal.
SE helps the nervous system find the balance, instead of being stuck in one extreme, to develop a resilient equilibrium (Baranowsky & Gentry, 2023; Kuhfuß, 2021; Brom et al., 2017; van der Kolk, 2015).
How somatic therapy retrains your nervous system
When someone's been living in chronic hyperarousal or freeze, their nervous system has essentially learned that this is the default setting. Somatic therapy has the power to help clients restore flexibility to a system that's gotten rigid and stuck, by moving from stuck to calmer and more regulated ways of being.
Through the process of repetitive embodied experiences, the system can be taught that it can come down from high alert. Each time a client practices noticing activation and finding their way back to regulation, they're creating new neural pathways and increasing neuroplasticity (Gorra, 2022; Kearney & Lanius, 2022; van der Kolk, 2015).
For trauma survivors, the body can become a dangerous place. Somatic therapy gradually helps clients discover their body can be a resource when there is increased ease, reduced reactivity to triggers, more flexible stress responses, and a growing sense that their body is on their side.
A “felt sense of safety" is when someone knows AND feels safe in their body. When the nervous system finally gets the message "the danger is over," it can stop running survival protocols and redirect that energy toward connection, growth, and living life (van der Kolk, 2015).
Somatic therapy for PTSD: results and timeline
Clients recovering from trauma often want to know "how long will this take?" While every person's timeline differs, there are patterns we see clinically. Somatic approaches can significantly reduce PTSD symptoms, but it's not usually a quick fix.
In most cases, clients start noticing shifts in hypervigilance within the first few months. The constant scanning for danger starts to soften and flashbacks decrease in both frequency and intensity, as the body learns it is in the present, not the past.
An example of a typical recovery timeline:
- 6-8 weeks: Clients begin to feel more grounded and notice that they can identify when they're activated.
- 2-3 months: Clients learn that noticing body sensations doesn't have to lead to overwhelm.
- 3-6 months: The window of tolerance expands—clients develop the capacity to ride the waves without drowning in them.
- 6-9 months: Clients are more consistently aware of internal states and better at reading body signals.
- 9+ months: Clients have reconnected with their body, trusting it as a resource and guide.
Recovery timelines often depend on how long the nervous system has been stuck in these patterns. Individuals recovering from multiple traumas may need a year or more of treatment.
When to consider somatic therapy
As a therapist, I look for two indicators that it's time to try somatic therapy: when traditional therapy hasn't fully resolved symptoms and when symptoms feel rooted in the body.
Here are a few examples from my practice that highlight how Somatic Therapy can expand on the work clients have already done.
- Sarah had done years of CBT work after a car accident and could understand rationally that driving was safe, but her body was still living in that moment of impact. Every time she got behind the wheel, her hands would shake, her heart would race. CBT had given her insight, but it hadn't reached where the trauma actually lived. Somatic Therapy helped her complete her response cycle to achieve more control over her body's sensations when in the driver's seat.
- Marcus had gained understanding of how childhood emotional neglect shaped his relationships. He could articulate the patterns beautifully. But he still couldn't feel his emotions—just chronic numbness punctuated by explosive anger because his body was still stuck in that childhood freeze response. Somatic Therapy helped Marcus recognize that numbness and anger were showing up in his body when he felt neglected in his adult relationships. Those sensations served as warning signs where Marcus could then choose different behaviors, drawing him closer in his relationships.
- David came in expressing chronic neck and shoulder tension that no massage or physical therapy could resolve. As we explored, it became clear his body was holding decades of hypervigilance from growing up with a father who abused alcohol. Somatic Therapy helped release the tension and create new neural pathways of feeling safe.
- Megan had constant low-grade anxiety living in her chest—tight, constricted, like she couldn't take a full breath. Turns out her body was holding patterns from childhood medical procedures. Her conscious mind had no real memory, but her body remembered. Using Somatic Therapy, Megan was able to locate her anxiety in her body and use SE to release it.
How to find a somatic therapist who can help with trauma
When looking for a somatic therapist for trauma, start by verifying core mental health credentials—look for LCSWs, LMFTs, LPCs, or psychologists with graduate-level training. If possible, consider working with a therapist who has a specialized certification in somatic experiencing, sensorimotor psychotherapy, or trauma treatment, such as a:
- Somatic Experiencing Practitioner (SEP)
- Certified Sensorimotor Psychotherapist
- Certified Clinical Trauma Professional (CCTP)
Therapist directories with advanced search filters allow you to search for licensed clinicians near you who take your insurance and specialize in somatic treatment for trauma.
References:
Baranowsky, A. B. & Gentry, J. E. (2023). Trauma practice: A cognitive behavioral somatic therapy (4th edition). Hogrefe Publishing Corporation.
Brom, D., Stokar, Y., Lawi, C., Nuriel-Porat, V., Ziv, Y., Lerner, K., & Ross, G. (2017). Somatic Experiencing for Posttraumatic Stress Disorder: A Randomized Controlled Outcome Study. Journal of traumatic stress, 30(3), 304–312. doi.org/10.1002/jts.22189
Gorra, N. (2022). The genetic and somatic expressions of trauma: A review of pathology and treatment. International Journal of Multidisciplinary Research and Growth Evaluation, 3(6), 290-297. doi.org/10.54660/anfo.2022.3.6.10
Kearney, B. E., & Lanius, R. A. (2022). The brain-body disconnect: A somatic sensory basis for trauma-related disorders. Frontiers in neuroscience, 16, 1015749. doi.org/10.3389/fnins.2022.1015749
Kuhfuß, M., Maldei, T., Hetmanek, A., & Baumann, N. (2021). Somatic experiencing – effectiveness and key factors of a body-oriented trauma therapy: a scoping literature review. European Journal of Psychotraumatology, 12(1). doi.org/10.1080/20008198.2021.1929023
Van der Kolk, B. (2015). The body keeps the score: Brain, mind, body in the healing of trauma. Penguin Books.
Feb 16, 2026

Looking for a therapist?
Get tips on finding a therapist who gets you.
By submitting this form, you are agreeing to Alma's privacy policy.



