Articles
The 5 Healthcare Trends Therapists Need to Know in 2026
Kate Mellor, Chief Commercial Officer at Alma, provides a clear, clinician-focused look at how payer trends and policy changes shape behavioral health—and what it means for your practice.

I’m Kate Mellor, Chief Commercial Officer at Alma. In every role that I’ve had throughout my career, I’ve sat between major stakeholders in healthcare. It’s my job to be a translator—to find the common ground. I do that now at Alma; I sit between the clinician community and payers, including insurance companies and employers. I try to speak both languages, because it’s my belief that with greater understanding, we can work together to create value.
Another key part of the work I do is tracking what’s happening in the larger healthcare space, finding those trends that could impact therapists in private practice, and helping to make strategic decisions to ensure that Alma can support you now and in the future. Our goal is to share information about those trends with you, so you can make informed decisions.
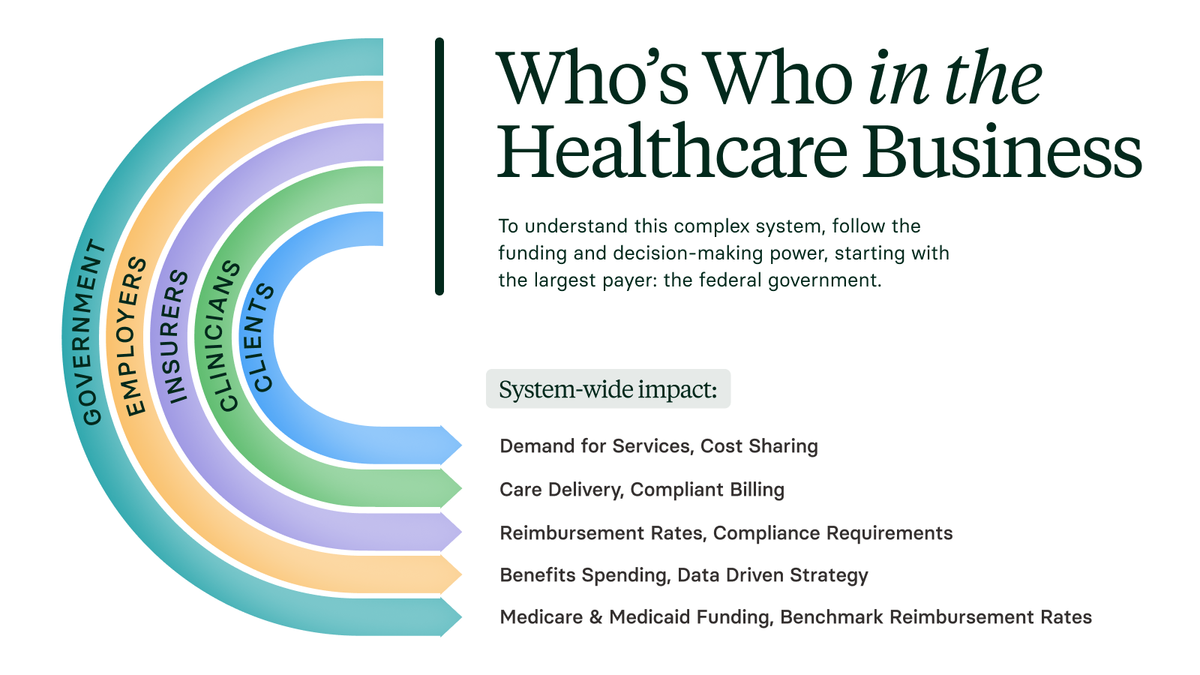
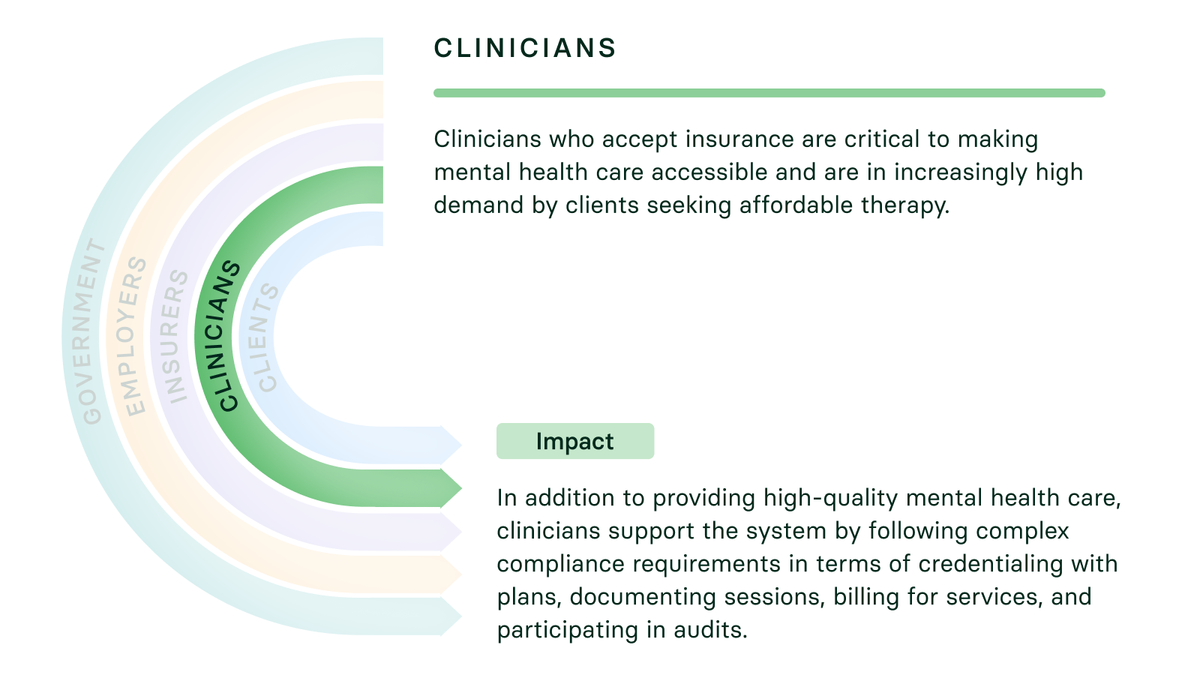
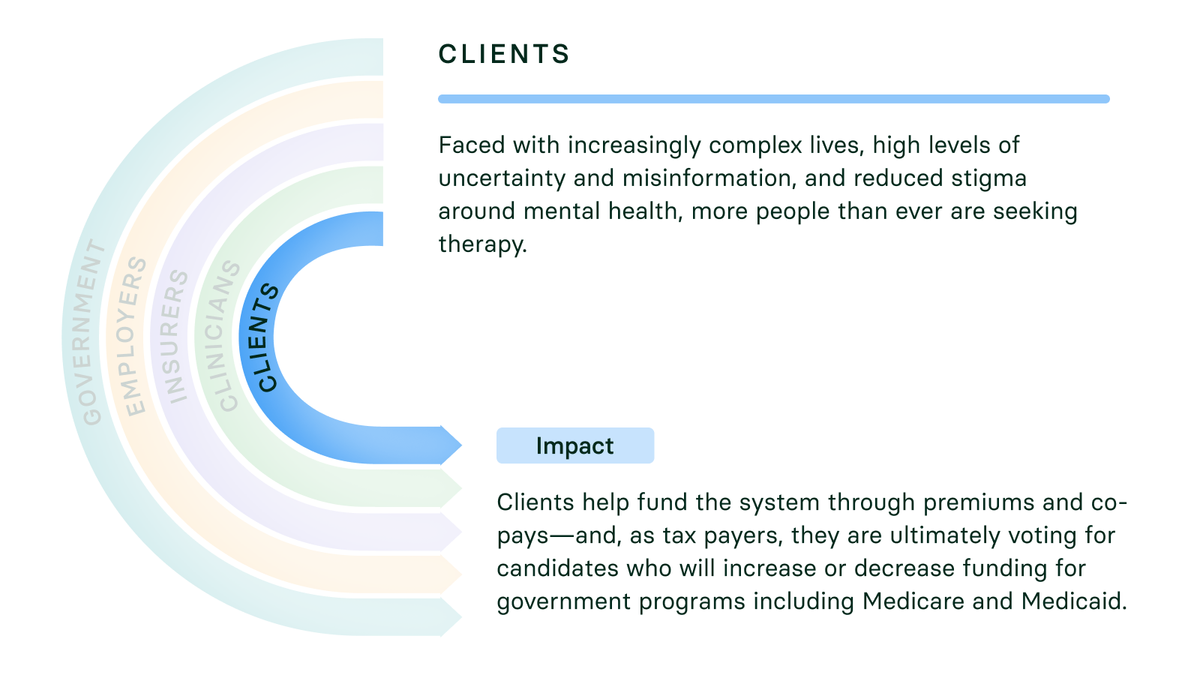
While you don’t need to know everything about the healthcare system to use that information, it does help to understand who the big entities are, what they care about most, and how the decisions they’re making can impact everyone in this system, most importantly you and your clients.
So, before we dive into the most important trends to be aware of now, let’s talk a little about this system that we’re all working within.
To understand the system, follow the funds
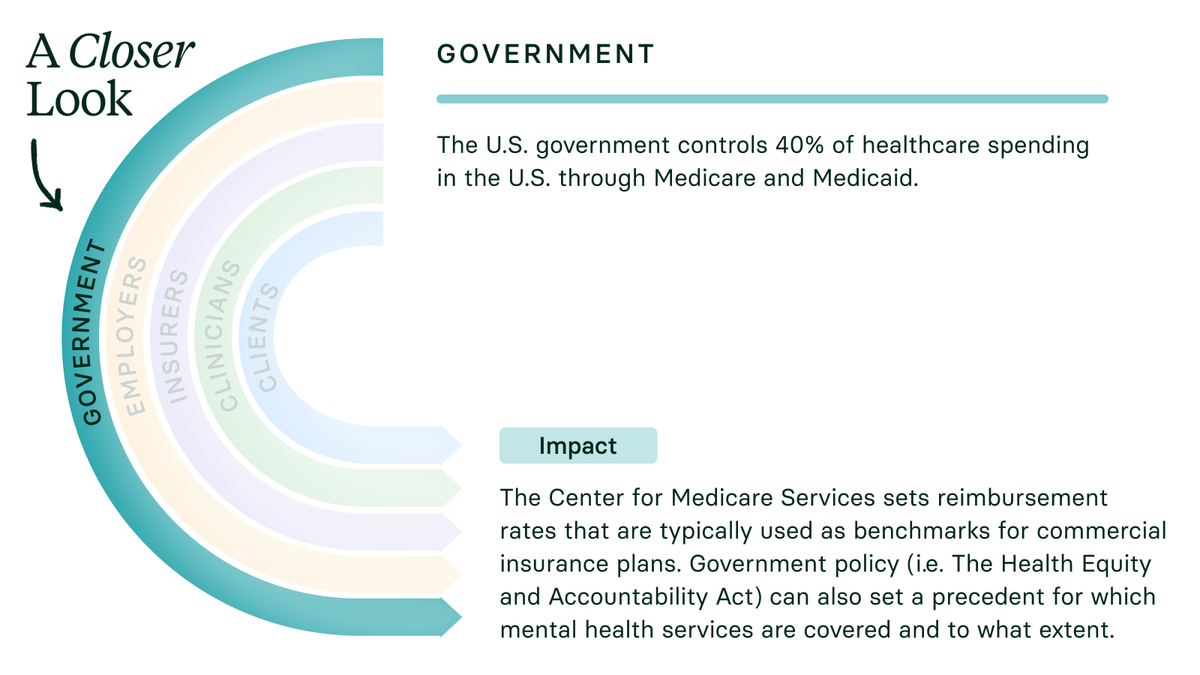
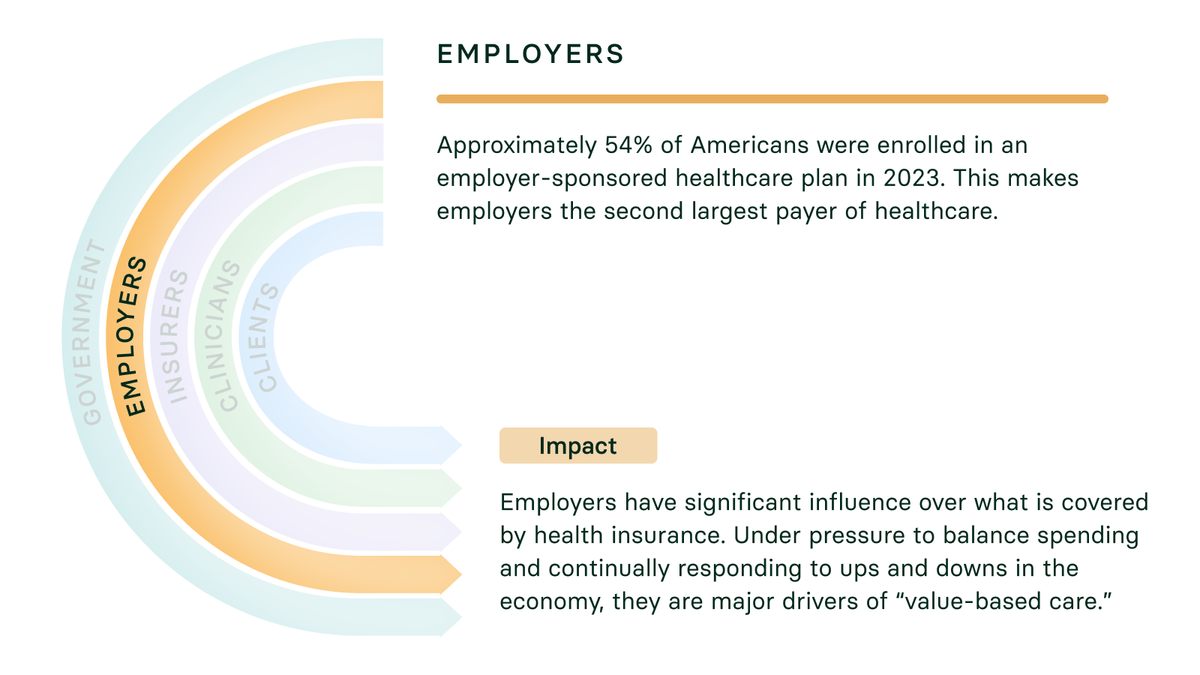
Healthcare in the U.S. is incredibly complex. To simplify it, consider who pays for care, starting with the two biggest payers: the federal government, through programs like Medicare and Medicaid, and the employers who pay for care for their employees.
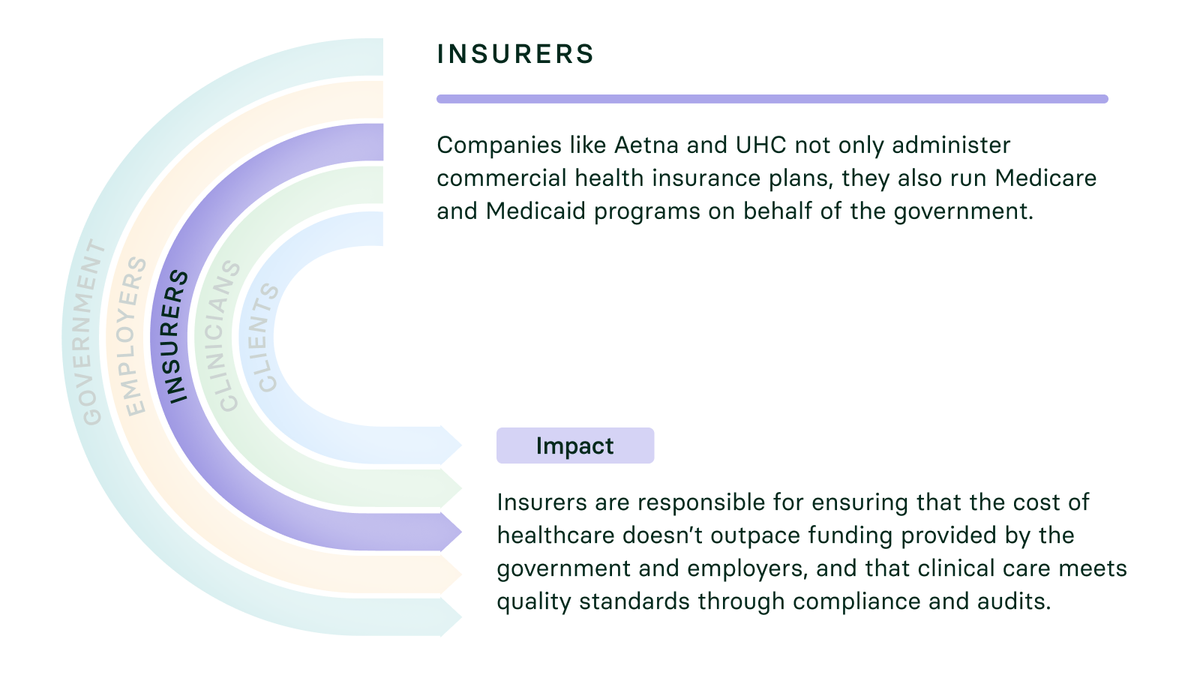
Commercial insurance companies like Aetna and United Healthcare are also payers, but these companies often act as subcontractors to the government administering programs like Medicare and Medicaid, and are responding to the needs of employers, who purchase their commercial insurance programs.
Together, the government, employers, and insurance companies are the entities making most decisions about how money flows. The following infographic will give you more detailed insight into their impact—and the impact of clinicians and clients on the wider system.
5 Trends transforming healthcare
Experts project that the healthcare system will change more in the next 10 years than it has changed in the last 100 years. With that in mind, I’m spending a lot of time listening to different voices in healthcare, especially employers, to track and project the direction of those changes.
Based on my research so far, here are some of the major healthcare trends that are already impacting the work you do—or very likely will in the near future—and how we're thinking about them at Alma.
1. Clinician-Led AI Tools
Experts agree that AI is poised to change the healthcare system as we know it. Today, there are so many systems and processes in healthcare that are highly manual in nature. Even just the way claims get paid by a payer—there’s a lot of people and process and lack of automation behind that. We’re going to see a massive shift in the automation of the administrative work that happens in healthcare.
AI is also going to start to impact the ways that providers show up for their patients. How do you need to communicate with your patient? When are you communicating? How is AI extending your ability to communicate with your patient at nine o’clock on a Saturday? You can expect to see a lot of change in that space as technology quickly advances.
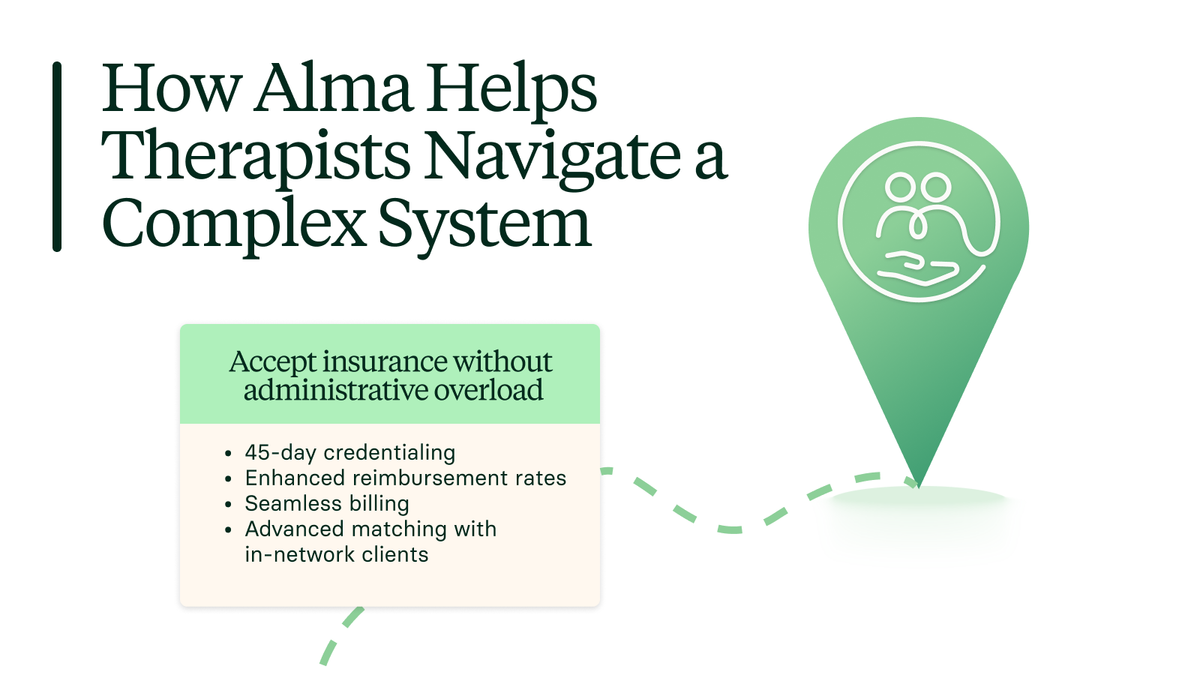
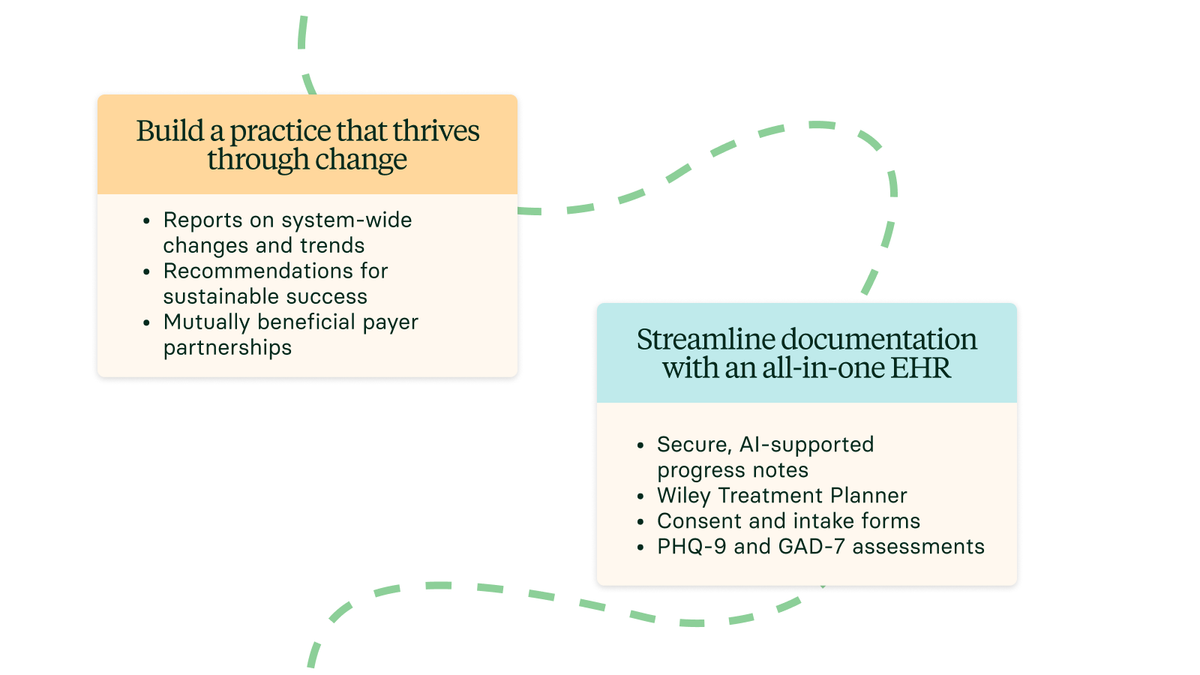
In thinking about how AI can be used with your patients, the team at Alma is making sure that providers can harness the power of AI and shape how it gets used in their practice. And so that’s why we’re focusing on clinician enablement, and making it easier to do the things you need to do every day in your practice, like take compliant progress notes and use medical coding.
2. “Primary Care Providers” for Behavioral Health
As discussed above, employers are making a lot of decisions about what gets covered and to what extent. In conversations with employers about mental healthcare, the thing that I hear talked about most is care navigation.
Care navigation for physical health is well established. Patients start with a primary care provider or PCP who knows their medical history and can refer them to the right care at the right time.
In mental health or behavioral health, as it’s also referred to, patients don’t have the equivalent of a PCP. This is problematic because there are now more people than ever before who have access to in-network mental health care as well as digital self-care and a wide range of other support services. The question is what to use when and why—as well as how different options work together.
So the challenge that employers are struggling with is that they feel like their employees don’t know how to navigate to the right care for mental health issues.
Ideally, individuals will feel I know where to start, and I have a guide. Maybe it’s a therapist who’s guiding patients along their mental health care journey in the same way that a primary care provider might guide a patient along their medical care journey. That’s something that we’re thinking a lot about at Alma and is likely to play into our long-term strategy.
3. New Coverage Under High-Deductible Plans
Legislation passed this summer changed the rules about what can get covered under high deductible plans. So for example, high deductible plans can now cover virtual visits, including virtual visits for behavioral health, without having to first meet a deductible, what’s often called first dollar coverage.
This is relevant because it has the potential to impact how employers design behavioral health benefits. Do you have to pay a deductible? Will you pay a smaller cost share? That in turn can influence what your clients might have to pay out of pocket.
Today Alma is part of many EAP networks with payers which are benefit plans—separate from medical coverage that offer therapy with no cost share. If medical plans can now also offer no cost share coverage, I think we’ll see some EAP 2.0 models emerge. And with our existing participation in the EAP space, we’ll be well positioned to work with any newly emerging models to support access.
4. Managing a System Under Pressure
A phrase you’re likely to hear more often is ‘utilization management,’ which is one way that insurance companies keep the system working when healthcare funding can’t keep up with the need for care.
A timely example is our aging population. It’s now the norm in the U.S. to live into your 80s or beyond. That means more and different types of services will need to be paid for, from home health aids to long-term medications.
Another example is the recent policy change that reduces the number of people eligible for Medicaid. With more uninsured people using the system, more bills will go unpaid. The downstream effects can include hospital closures in rural areas and hospital systems closing that gap by charging payers more for commercial plans.
Payers and even the federal government are trying to figure out how do we afford all this? This is pressuring them to ‘find savings’. As a provider, you may have already noticed this pressure in the form of payers requesting more detailed documentation or questioning the use of certain codes.
At Alma, we have regular working groups with payers to better understand their documentation requirements so we can guide you in your practice—similar to how a GPS navigation system may tell you there is speed check ahead. By building our expertise on payer-specific guidelines, we can help you ensure compliance.
5. Making it Easier to Measure Outcomes
Outcomes measurement is another major area of focus for payers. Employers, who need to make sure that their limited benefits dollars are being well spent, often ask the insurance companies they work with, How can you show me that the care that I'm paying for—whether it’s therapy or any other type of care—is helping to make people better? It's insurance companies' job to be able to answer that with data.
At the same time, payers are willing to reward providers for things that they perceive as high value, things that they perceive as making people better and taking stress out of other parts of the system. So payers are increasingly expecting that data as a way to demonstrate value to justify premium rates.
This is why we’re engaging in outcomes measurement at Alma. We’re already working to provide payers with the data they need in a way that is HIPAA compliant and doesn’t put added strain on providers.
Why partnership matters
One of the many things that makes Alma different from competitors is our focus on partnership. The partnership between Alma and the clinicians in our community and the partnership between Alma and payers. I think that when you deeply know your partner, you can understand what motivates them and then you can find ways to create value based on what’s important to each of you. (I’m sure the couples therapists reading this will have something to add here.)
And so in payer relationships, we focus a great deal on understanding where payers want to create value and then figuring out ways to deliver value for payers in such a way that providers also win.
For example, one of the challenges that payers struggle with is creating digital directories that successfully help people find in-network care. And so over the the last two years, we’ve built a number of integrations with payer directories where consumers can find and schedule care in the moment with in-network Alma providers.
Clinicians, in turn, can connect with the right patients. This is a great example of Alma knowing a business objective that our partners want to achieve, and figuring out how to do it with technology in a way that also benefits our provider community.
Our mission is clear
One of the things I love about my journey here at Alma is I feel like I’ve had a front row seat to these massive changes in healthcare. And I think the first one was COVID. I think that you can’t underestimate the impact on COVID for the behavioral healthcare community. Every day, I am astounded by how as a community of behavioral health therapists was able to go from delivering 95% of their care in person to delivering 95% of their care digitally through virtual platforms like Alma.
I’m incredibly proud to have the opportunity to use my expertise on the payer side to help providers navigate change in the past and in the future. In many ways we find ourselves at the next crossroads in healthcare. Alma is here to advocate on your behalf and provide you with a seat at the table, so you can help steer this transformation and ensure it happens in a way that’s focused on you and your priorities.
Take action:
Achieve sustainable success
Alma helps clinicians thrive through change. Get the support you need to build a sustainable private practice that meets your professional and personal goals.

Written by
Kate Mellor, Chief Commercial Officer at Alma
Learn More
Build a thriving private practice with Alma
We believe that when clinicians have the support they need, mental health care gets better for everyone.


