
Unpacking Gut Health and Anxiety: The Mind-Body Connection
If you’ve ever felt anxiety in your stomach, you’re not imagining it. Here’s how addressing both your mind and body can help you feel better overall.
Here’s what’s becoming increasingly clear from the latest research: your gut really does have a mind of its own, and it’s been communicating with your brain all along. This constant dialogue, called the gut-brain axis, means that what’s happening in your digestive system isn’t separate from your mental and emotional state, it’s intimately connected to it.
One of the most encouraging parts? Understanding this connection opens up a new avenue for relief that many people with chronic digestive issues like irritable bowel syndrome (IBS) have yet to explore: working with a mental health therapist who understands how conditions like anxiety can impact your gut.
It’s not about your symptoms being “all in your head,” it’s about recognizing that your head and your gut work in tandem, so when you treat both your mental and physical health, you can see significant improvements that treating either one alone can’t achieve.
Let’s take a deeper look at the gut-brain axis, how it works, and whether seeing a mental health therapist for your gut issues is a good option for you.
What is the gut-brain axis?
A massive amount of information flows between your brain and your gut. This constant communication is called the gut-brain axis, and it plays a vital role in regulating both physical and emotional well-being. If you’ve ever had “butterflies in your stomach” before a date or had a “gut feeling” about a decision, you’ve felt this connection in action.
Scientists theorize that this close relationship developed because nutrition and digestion are so fundamental to our survival. Early humans needed their brains to stay closely attuned to what they were eating to get enough fuel and to rapidly detect if something was harmful. Over time, this system evolved into an intricate network of nerves, hormones, metabolites, and immune signals that tightly link the gut and the brain.
How the gut and brain communicate
The gut-brain axis operates through several overlapping systems that send and receive information in real time. Three major components are the vagus nerve, the enteric nervous system, and the gut microbiome.
The vagus nerve
A pair of long nerves that run from your brainstem through your chest and into your abdomen. The vagus nerve helps regulate digestion, blood pressure, heart rate, breathing patterns, immune responses, and aspects of stress and emotional regulation, and other involuntary body functions. Signals constantly travel both ways along this nerve, meaning your brain can influence your gut and your gut can influence your brain.
Enteric nervous system
Aside from the brain and spinal cord, the enteric nervous system is the most complex neural network in your body, with roughly 200–600 million neurons. It helps coordinate swallowing, enzyme release, nutrient absorption, blood flow, and waste elimination, all without conscious thought.
The enteric nervous system doesn’t generate thoughts or emotions, but it is in constant communication with the brain. This two-way communication influences how we feel, think, and respond to stress. The ENS can also operate independently: it can detect a problem with your digestion and address it directly without involving your brain.
Gut microbiome
The “gut microbiome” refers to the trillions of bacteria, viruses, and fungi that live in your digestive tract. These microbes support metabolism, immune function, and the production of signaling molecules that influence gut cells and vagus nerve signaling. They also help to create the neurotransmitters (like serotonin and dopamine) that send messages between your brain and your digestive system.
In fact, about 90% of your body’s serotonin—a chemical essential for mood regulation—is produced in the gut. This is why many SSRIs (Prozac, Zoloft, etc.) initially cause digestive upset. As SSRIs increase serotonin production, serotonin receptors in your gut become stimulated, changing how quickly food moves through your digestive tract. (This side effect usually dissipates as your body adjusts to the medication.)
There is a lot more to understand about how specific microbes influence mood and cognition, but studies show that disturbances in the microbiome (dysbiosis) are associated with changes in stress responses and with several mental health conditions.
What is the connection between gut health and mental health?
Researchers long assumed that people with digestive disorders were more likely to experience anxiety and depression simply because of the stress of living with those conditions. And while managing a digestive condition is really challenging, research increasingly supports the idea that disturbances in the gut can contribute to the development and intensity of mental health disorders.
It works the other way around, too. Anxiety, panic, depression, and other forms of emotional distress can disrupt digestion, alter gut motility, and change the composition of the microbiome. Together, this can create a snowball effect where both systems fall out of balance.
For example, imagine that you are feeling anxious about a big presentation. That anxiety can trigger your body’s “fight-or-flight” response, leading your body to release cortisol and adrenaline. These hormones divert blood flow away from digestion to prioritize dealing with the perceived “threat.” This physiological shift can cause nausea, cramping, constipation, and diarrhea… which means you’re now running to the bathroom on top of feeling stressed about your presentation. Not helpful!
Which mental health conditions or symptoms may be related to the gut-brain axis?
Researchers suspect the gut-brain connection plays a role in a wide range of physical and mental conditions. Here are just a few examples, starting with gut issues:
Digestive conditions
- Irritable bowel syndrome (IBS)
- Gastroparesis
- Functional dyspepsia
- Functional dysphagia
- Infant colic
Mental health conditions
- Anxiety and depressive disorders
- Chronic stress
- Chronic fatigue
- Visceral hypersensitivity
Pain-related and neurological conditions
- Noncardiac chest pain
- Nerve-related pain (e.g., multiple sclerosis)
- Chronic pain
- Autism
- Parkinson’s disease
The benefits of combining mental health care and gastrointestinal medicine
Because the gut-brain connection is bidirectional, addressing both ends of the gut-brain axis can be especially effective for people living with digestive issues. This integrated approach can help patients break the vicious cycle of emotional distress and gut distress, leading to longer-lasting symptom relief. In addition to finding a great doctor/gastroenterologist, a gastrointestinal psychologist could be a transformative member of your care team.
A gastrointestinal psychologist is a licensed psychologist trained to address the emotional and neurological factors that influence digestion. They use evidence-based techniques to help patients manage anxiety, regulate the stress response, and improve their relationship with their bodies to reduce digestive symptoms. If you can't find this kind of specialist in your area, consider searching for a therapist that specializes in working with chronic illness or the mind-body connection.
Some evidence-based therapeutic approaches for people with digestive conditions include:
Cognitive Behavioral Therapy (CBT): Helps reframe thought patterns that contribute to stress-related gut symptoms. Gastrointestinal-CBT is a short-term therapy specifically designed to connect how you think, feel, and behave in the context of your gastrointestinal condition.
Gut-Directed Hypnotherapy: Uses relaxation and visualization techniques to reduce gut sensitivity and pain. One clinical trial of 1,000 patients showed that over 75% of patients achieved a clinical response to hypnotherapy. There were also significant improvements in anxiety and depression scores.
Mindfulness-Based Stress Reduction (MBSR): Improves body awareness and reduces anxiety-driven flare-ups.
Biofeedback: Uses sensors to measure things like muscle tension, heart rate, or skin temperature, so you can learn to consciously control certain physiological responses. It can be especially helpful for managing pain or stress-related symptoms.
Acceptance and Commitment Therapy (ACT): Works toward building a meaningful life while accepting the things you can’t change. ACT helps people to clarify their values (like connection, creativity, or service) and find ways to honor them within their current reality.
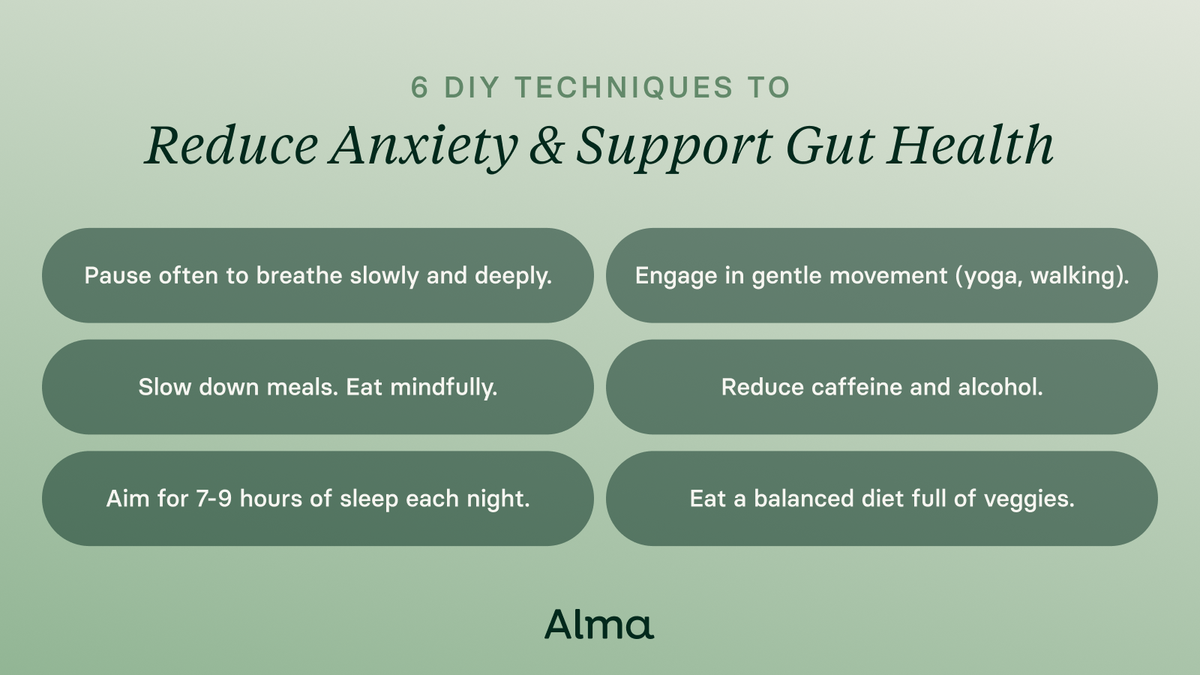
DIY techniques to reduce anxiety and support gut health
You don’t need to wait to begin therapy to start supporting your gut-brain connection. Everyday practices can help you reduce stress and improve digestion. These practices will no-doubt sound familiar, because they’re recommended by most doctors to improve overall health: Breathe deeply, take walks, eat mindfully, limit caffeine and alcohol, get your rest, and eat a fiber-rich diet that contributes to a healthy microbiome.
Key takeaways
Your gut and brain are in constant dialogue. Treating digestive issues can improve your mental health, and addressing anxiety, stress, and emotional well-being can also reduce digestive symptoms.
Understand your gut-brain communication through therapy
A growing body of research supports combining traditional gastrointestinal care with mental health therapy. Seeing a therapist who understands this critical connection can help you strengthen the communication between your gut and brain, leading to improved mood, fewer digestive symptoms, and a greater sense of overall well-being.
Nov 21, 2025

Looking for a therapist?
Get tips on finding a therapist who gets you.
By submitting this form, you are agreeing to Alma's privacy policy.




